Research Project Imaging bronchial team
Group leader François Laurent
 |  |  |  |
|---|---|---|---|
 |  |  |
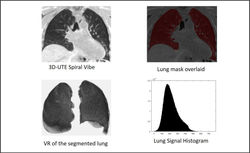
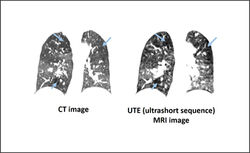
CT scan is the most commonly used imaging modality for imaging chronic inflammatory bronchial disease i.e. COPD, asthma and cystic fibrosis. CT complements spirometry, a global measure of the presence of the disease by providing anatomic localization, characterizing emphysema, evaluating airway and vascular disease and several extrapulmonary manifestations of the disease. CT provides quantitative metrics that have been tested as markers for disease progression, prediction of exacerbations and identification of phenotypes. Quantitative phenotyping can be provided in the lung parenchyma, medium and large and small airways by measuring several metrics used to estimate airway size or expiratory gas trapping, vascular component by measuring main pulmonary artery/ascending aorta ratio and cross sectional areas of small vessels. Chest CT is also able to provide extrapulmonary disease especially in COPD, considered today a multisystemic disease: coronary calcium scoring as a cardiovascular disease marker, skeletal muscle dysfunction and muscle wasting and increased risk of osteoporosis by estimating bone mineral density. Artificial intelligence (AI) includes supervised and unsupervised metrics as well as deep learning methods for disease quantification and subtyping. We have hypothesized that advanced CT scan analysis quantitative data and AI methods would allow to better define the phenotype chronic inflammatory bronchial disease and objectively measure changes brought by therapies. Magnetic Resonance Imaging (MRI) is a radiation-free technique which has been demonstrated to add meaningful functional information that cannot be reached using CT. Recent advances in 3-dimensional ultra-short echo time (3D-UTE) imaging have been shown promising to improve lung MR imaging quality. The combination of pulse sequence may rather benefit from the potential of MRI to get more complete insight into inflammatory processes by combining several contrasts, as compared to other ionizing methods. MRI has been shown promising in assessing lung changes and mucus load with high resolution, without any contrast agent, and ventilation-perfusion mismatch. Therefore, lung MRI could be proposed as a radiation-free imaging biomarker suitable for repeated follow-up of patients during clinical trials. Quantitative data can be provided on MRI as well as with CT for various components of lung. We have hypothesized that MRI combining various sequences and quantification can provide a objective tool for phenotyping and follow-up chronic bronchial diseases
